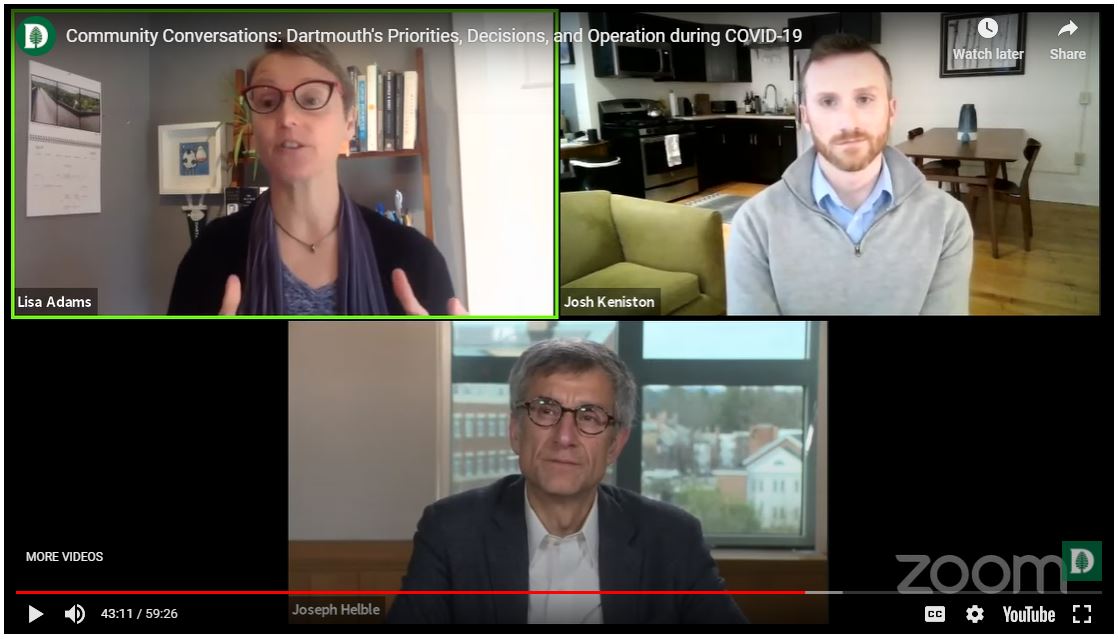
Geisel Associate Professor Lisa V. Adams, MD, MED’90 (top left) co-chairs Dartmouth’s COVID-19 Task Force with Josh Keniston, vice president of campus services.
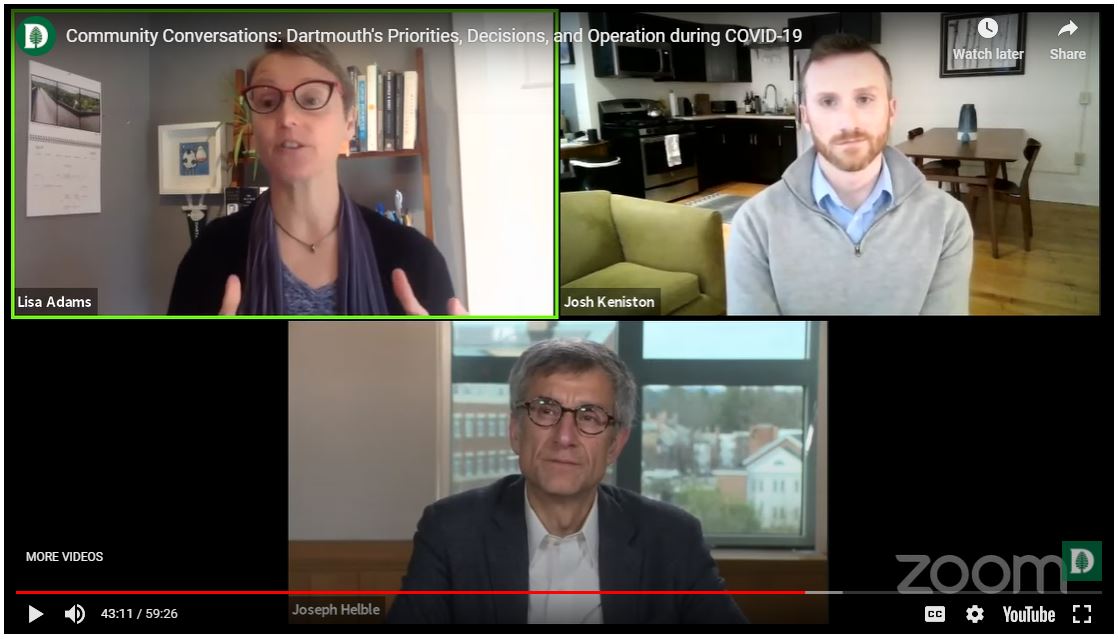
Geisel Associate Professor Lisa V. Adams, MD, MED’90 (top left) co-chairs Dartmouth’s COVID-19 Task Force with Josh Keniston, vice president of campus services.
When new and dangerous illnesses emerge, scientific discovery and innovation are needed at every level. At the same time, the people and systems responding to the crisis must be well informed, well supported, and resilient.
This is where Geisel excels: at the intersection of biomedical discovery, innovation, healthcare delivery science, and the training of wise healthcare leaders.
In fact, discoveries made in a Geisel lab are being used in the newly approved COVID-19 vaccine from the Pfizer/BioNTech partnership. Read more about the research that made the vaccine possible.
Below is a sampling of the many ways that Geisel faculty, students, staff, and alumni are responding to the COVID-19 pandemic.
Validation of rapid, low-cost COVID-19 test
In spring 2020, Geisel scientists collaborated with a Dartmouth-Hitchcock pathologist to validate and adapt for widespread use a rapid, low-cost COVID-19 diagnostic test from Atila Biosystems. The Atila test can produce results in less than one hour and received emergency use authorization from the FDA in April, based on results from Geisel. The test is now being used in the U.S. and in many low-resource countries, including El Salvador, Peru, Guatemala, Nigeria, India, Angola, and South Africa.
Read more about this COVID-19 test.
Novel COVID-19 diagnostic test
The Dartmouth-Hitchcock Laboratory for Clinical Genomics and Advanced Technology, led by Geisel professor Gregory Tsongalis, PhD, was one of the first non-governmental labs in the country to begin testing people for the new coronavirus. Its test came online March 18, 2020. The lab has the surge capacity to process 1,000 COVID-19 test samples in 24 hours and has partnered with the State of New Hampshire reduce the state’s backlog of tests and keep pace with surveillance testing at long-term care facilities.
Wastewater monitoring for early detection
Two assistant professors of pathology and laboratory medicine, Isabella Martin, MD, and Jacqueline Hubbard, PhD, are leading a collaboration between Dartmouth-Hitchcock, Dartmouth College, and several cities in New Hampshire to monitor wastewater for COVID-19. Between 40% and 65% of people shed the virus in their stool as much as a week before any symptoms—so this strategy could help administrators and public health officials identify and isolate infected persons to prevent community outbreaks.
Analyzing antibody responses to inform treatments
Researchers from Geisel, Thayer School of Engineering, a biotech firm, and the Universtiy of Texas-Austin are collaborating to study the breadth of antibody responses in patients who have recovered from COVID-19 and individuals who have not had the disease but have been exposed to other types of coronaviruses. Together, they are working on profiling and isolating the most effective of these antibodies for use as therapeutics and to inform potential vaccine efforts.
Antibody responses, inflammation, and age
Geisel immunologist and Cancer Center member Paul Guyre, PhD, is studying the increased prevalence of severe disease in COVID-19 patients over age 60. Antibodies acquired from lifetime exposure to other coronaviruses may cross-react with SARS-CoV-2 in a way that actually worsens infection and lung inflammation. He is also investigating the potential for human plasma to neutralize SARS-CoV-2 infection.
Health Equity and Rural Empowerment Initiative
In spring 2020, faculty and students at Geisel collaborated with colleagues at Dartmouth-Hitchcock, Colby-Sawyer College, local governments, and organizations across multiple regions of Northern New England to conduct an initial rapid study to do the following: identify rural health equity issues related to COVID-19; describe needs and solutions across the region; and identify areas for additional community-responsive research.
Mapping vulnerable regions
Collaborating with Microsoft Healthcare NeXT and CareJourney, researchers at The Dartmouth Institute for Health Policy and Clinical Practice are mapping the geography of COVID-19 vulnerability in the U.S. They are documenting regions with the greatest fraction of vulnerable people, using interactive heat mapping to assess the spread and growth of diagnosed cases using Hospital Referral Regions, and tracking real-time incidence and outcomes of hospitalized COVID-19 patients from about 250 hospitals nationwide.
Read more about TDI and COVID-19 mapping.
Telehealth regulatory changes
Faculty at The Dartmouth Institute for Health Policy and Clinical Practice collaborated with colleagues at Harvard Law School to document some of the most significant telehealth regulatory changes that have occurred in response to COVID-19—including payment, privacy, and licensing. They also summarized the views of key opinion leaders in telehealth and outlined the opportunities and challenges facing the healthcare system as it works to successfully harness the expanded role recently given to telehealth.
Read the academic paper on telehealth.
Geisel has prepared thousands of physicians, scientists, and healthcare professionals to take on the world’s biggest challenges. Here are just a few of the remarkable alumni who are leading responses to COVID-19.
Daniel Lucey, MD, MPH, D’77, MED’81
Senior Scholar, Georgetown University
Fellow, Infectious Disease Society of America, Global Health Committee
Research Associate, Anthropology, Smithsonian Museum of Natural History
Anne Schuchat, MD, MED’84
Principal Deputy Director
Centers for Disease Control and Prevention
Tenagne Haile-Mariam, MD, D’83, MED’88
Emergency Medicine Physician
George Washington University Hospital and United Medical Center
Peter Kilmarx, MD, D’83, MED’90
Deputy Director, Forgarty International Center
National Institutes of Health
Lisa V. Adams, MD, MED’90
Co-Chair, Dartmouth COVID-19 Task Force
Director, Center for Global Health Equity
Geisel School of Medicine at Dartmouth
Benjamin Chan, MD, MPH’13
State Epidemiologist, New Hampshire
